Pharmacy house calls? Get your prescriptions mailed directly to you.
Save yourself a trip to the pharmacy by enrolling in mail order delivery for your long-term medications.
Employees and their families enrolled in an Anthem-administered health plan (CU Health Plans Exclusive, Extended or High Deductible) have the option to receive 90-day supplies of maintenance drugs through the CVS Caremark Mail Order Pharmacy.
Many plan members have already taken the necessary steps to move their long-term prescriptions to a designated CVS pharmacy as a result of new pharmacy changes this plan year (which began July 1). Members have another option — skip the trip to the pharmacy and use mail order to have your next refill delivered directly to your door instead.
You can even temporarily change your delivery address in case you’re away from home for your next refill by adding an ‘alternate’ address to your profile for mail order. This includes setting an effective and expiration date for when the alternate address is to be used. Members can set this up in their online account or call CVS Caremark Customer Care (see "Reach out for help” section below) who can assist members in getting an alternate address set up.
How to get your mail order deliveries set up
Mail order service is only available for 90-day supply prescriptions. Plan members who have a shorter-term maintenance prescription will need to fill their prescriptions at a physical CVS pharmacy location. Short-term prescriptions like antibiotics can be filled at any participating pharmacy in the CVS Caremark network, including most major supermarkets and chain pharmacies.
CU’s CVS Pharmacy webpage features a chart that outlines pharmacy types and the prescriptions categories that can be filled at each. To find a pharmacy near you, use the CVS Caremark app or visit caremark.com, sign in to your account, open the Plan & Benefits menu, and select Pharmacy Locator to search for a nearby pharmacy.
For those members with long-term prescriptions that can be filled in 90-day supplies, you can set up mail order delivery in three ways.
- Through your doctor’s office — The easiest method, especially for new maintenance prescriptions, is to notify your prescribing doctor’s office to submit your prescription to CVS Caremark Mail Service Pharmacy. For electronic prescription submissions, they’ll select CVS Caremark MAILSERVICE Pharmacy, One Great Valley Blvd, Wilkes-Barre, PA 18706.
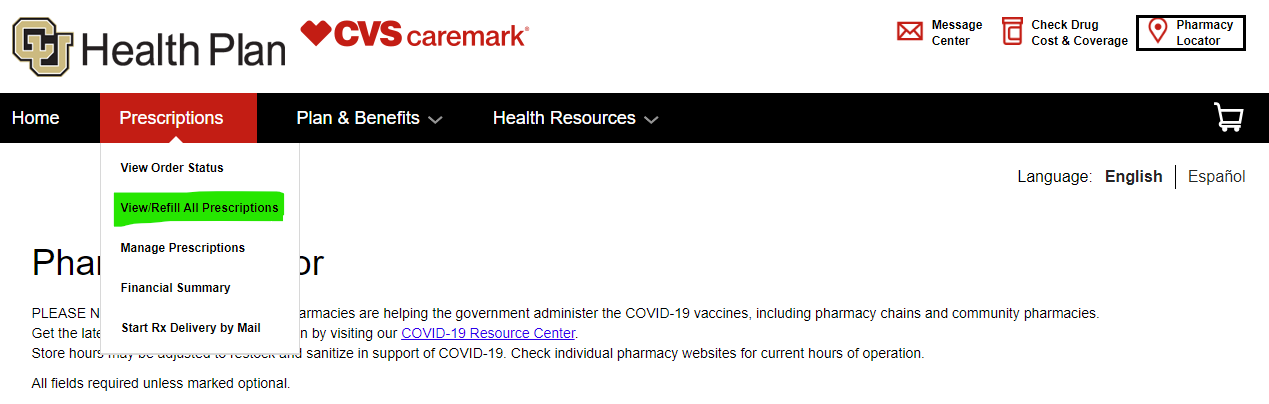
- Online through your CVS Caremark account — To set up your mail order fulfillment online, log in to your CVS Caremark account (or create an account if you haven’t already) through the CVS Caremark website. It’s best to take this step when you’re nearly due for a refill. Once logged in, select Prescriptions in your account menu and then choose Start Rx Delivery by Mail from the drop-down menu.
From there, you can search for your medication by name or scroll down further to see a list of your current prescriptions. When you see the medication to be filled by mail order, click Price this drug to the right of the drug name and follow the instructions to submit a request to fill that prescription by mail. Note: You may receive an alert message if it’s too soon to refill that specific drug. Try again closer to your refill window. - By phone with CVS Caremark Customer Care — You can call CVS Caremark Customer Care at 1-888-964-0121 to request that CVS Caremark contact your doctor for a new prescription.
Mail order medications will arrive within seven to 10 business days, barring the need for any prior authorization from your doctor’s office.
Automate your refills
Once your mail order delivery is established, you can initiate your refills online through your CVS Caremark account, by text message or through automatic delivery.
To set up automatic refills, log in to your CVS Caremark account and choose Prescriptions from the menu, then select Manage Automatic Refills. Some drugs, including controlled substances and specialty medications, cannot be set up for automatic delivery.
To refill your prescriptions manually, log in to your CVS Caremark account and choose Prescriptions from the menu, then select View/Refill All Prescriptions and select the eligible medication(s) to start your refill.
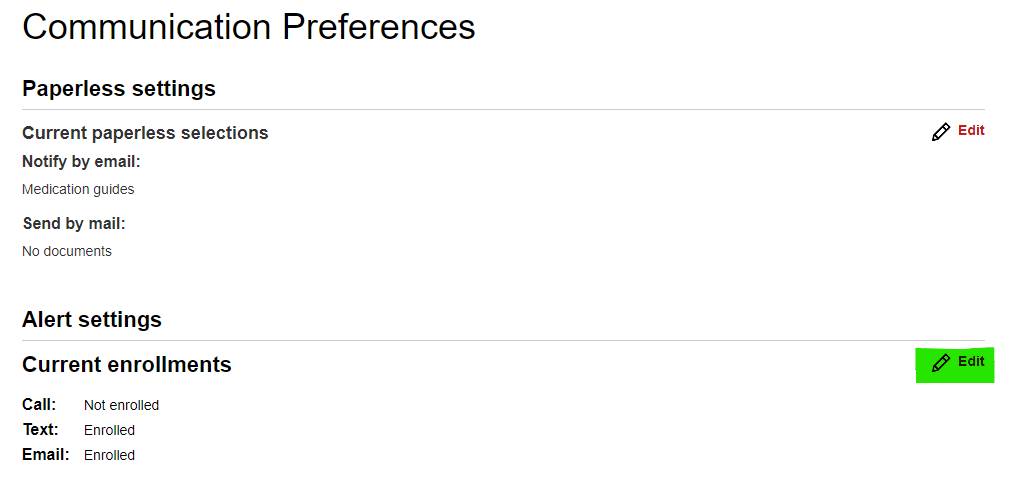
To refill your prescription by text message, sign up for text message alerts through your CVS Caremark account. Click on Profile at the very top, right-hand side of the page.
Under Update My Profile, select the Communication preferences link.
Under the “Alert Settings” heading, you’ll see a subheading of your “Current enrollments” with a very brief overview of your phone, text and email enrollments. Click the Edit link to the right of “Current enrollments” to see all your communication options.
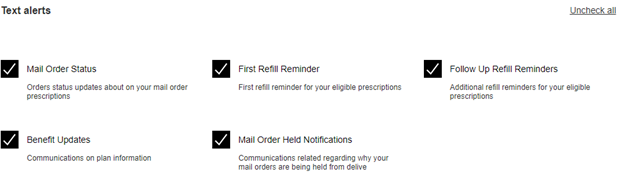
Under the “Text Alerts” section, click on the checkbox next to the text message alerts you wish to receive. To enable mail order refills by text, check “Mail Order Status,” “First Refill Reminder” and “Follow Up Refill Reminders” at minimum. Be sure to verify that the phone number they have listed for you is accurate and able to receive text messages. If it’s incorrect, scroll further down the page to edit your contact information.
Once your refill reminder texts are enabled, you will receive an automated text message alerting you when a medication is eligible for refill and instructions to authorize the refill.
Reach out for help
If you have difficulty establishing mail order delivery, reach out to the CVS Caremark Customer Care line (instead of your local pharmacy) at 1-888-964-0121; CU Health Plan-dedicated CVS Caremark Customer Care representatives can help answer specific questions about your plan coverage.
Contact CVS for:
- Questions about coverage or prescription costs.
- Assistance filling three grace 30-day refills before moving to a 90-day supply via mail order to CVS pharmacies.
- Assistance locating pharmacies that supply your medications.
- Assistance updating prescriptions with your medical provider.
If you have questions or concerns about your plan enrollments, obtaining ID cards or resolving issues that are taking longer than expected, you can reach out to Employee Services benefits professionals at 1-303-860-4200, option 3.






Add new comment