Anthem members can fill maintenance medications at Kroger pharmacies beginning April 1
Effective April 1, 2024, CVS Caremark will expand the Maintenance Choice network nationally to include Kroger-affiliated pharmacies, such as King Soopers and City Market pharmacies. The Maintenance Choice network comprises pharmacies where Anthem plan members can fill their long-term maintenance medications, in 90-day supplies, and have them covered by CVS Caremark.
CVS Caremark administers prescription drug coverage for all Anthem-administered CU Health Plans (the Exclusive, Extended, High Deductible, and Medicare). Enrolled members taking long-term maintenance medication must fill their prescriptions at specific pharmacies. For any newly prescribed maintenance medications, members are allowed three refills at any pharmacy in the broader CVS network before prescriptions must be transferred to a Maintenance Choice pharmacy.
Pharmacies available to CU Health Plan members to fill maintenance medications include:
- Kroger-affiliated pharmacies.
- Costco and its mail pharmacies (except Costco locations in Oklahoma and West Virginia).
- CVS Pharmacy (including those inside Target locations).
- CVS Caremark Mail Service Pharmacy
Collectively, the pharmacies listed above are part of the Maintenance Choice network. In Colorado, Kroger-affiliated pharmacies include King Soopers and City Market pharmacy locations comprising 148 stores within the state. CU Health Plan members residing outside of Colorado may have additional options through Kroger’s affiliated stores, such as Fred Meyer, Ralphs, and Kroger Food and Drug.
Please note: This list is accurate at the time of distribution and may be subject to change at any time.
Locate a Maintenance Choice pharmacy
CU Health Plan members who take maintenance medications must fill prescriptions in 90-day supplies at a Maintenance Choice pharmacy.
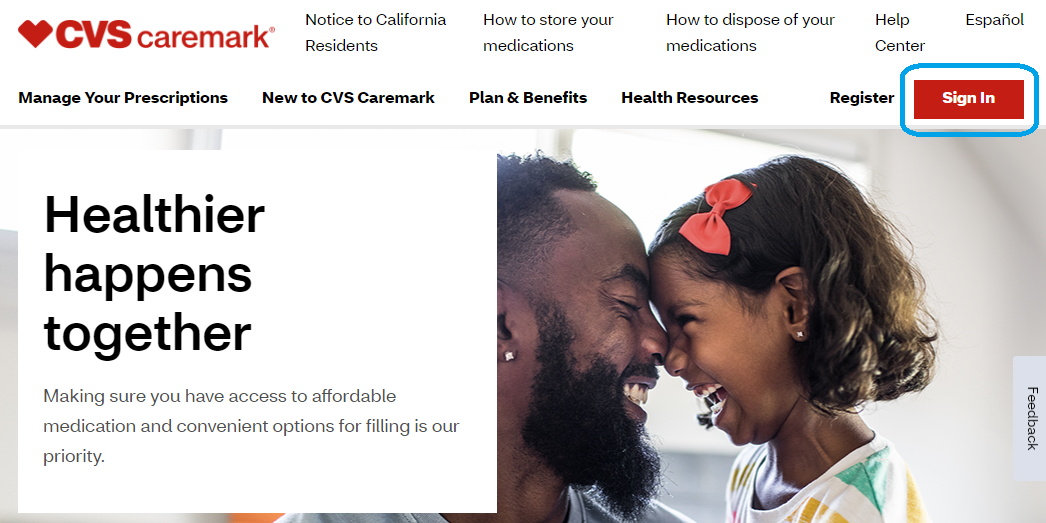
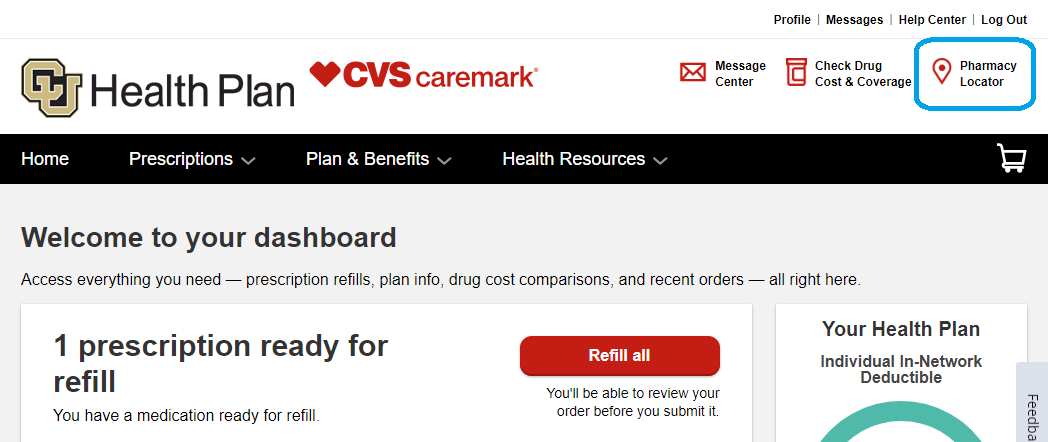
To find an eligible pharmacy, use the Pharmacy Locator Tool in the CVS Caremark app or in the online member portal at Caremark.com. The screenshots below are of the Caremark.com portal as viewed on a desktop computer.
1. In the member portal, select the “Sign in” button near the top right of the page.
2. After logging in, select the “Pharmacy locator” link near the top right of the page.
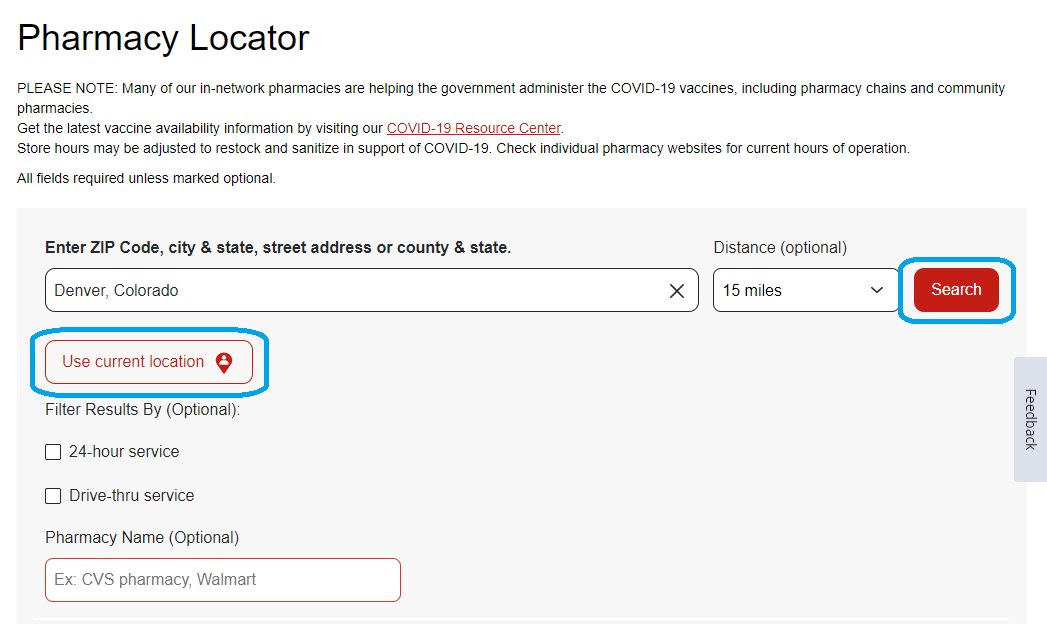
3. Enter your search location, select your distance range preference from the drop-down menu, then click the “Search” button.
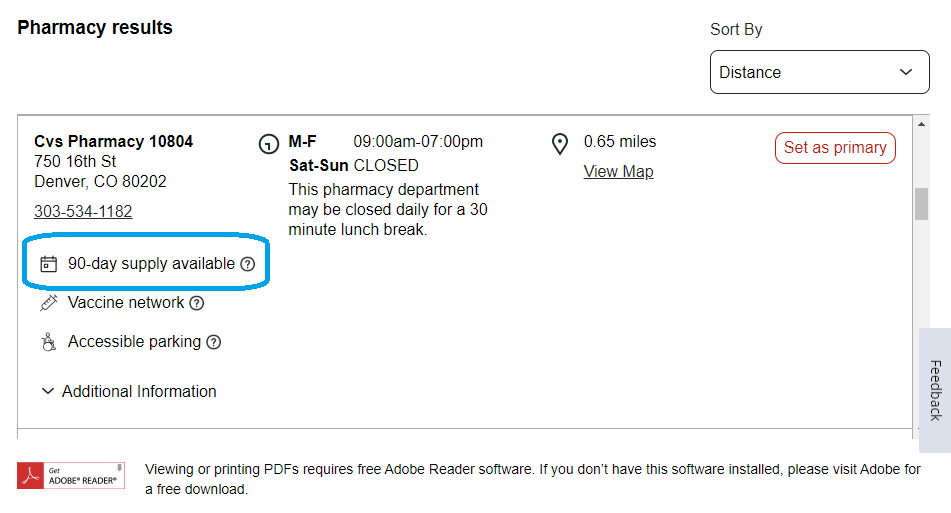
4. To identify Maintenance Choice pharmacies in your search results, look for a small calendar icon that says “90-day supply available” in the pharmacy description. For Kroger pharmacies, this icon will display starting April 1.
If you currently have maintenance medications filled at a non-participating pharmacy, read the CVS Caremark pharmacy benefits blog post for instructions to move your medications.
You can find instructions on establishing mail order delivery of your maintenance medications through CVS Mail Service Pharmacy. Mail order service provides convenient service options, such as email and text alert refill reminders and automated refills.
Have questions?
See the Employee Services pharmacy webpage for details on where to fill prescriptions, including short-term and specialty medications.
Call CVS Caremark Customer Care: 1-888-964-0121
Employee Services recommends calling CU’s dedicated CVS Caremark Customer Care line (instead of your local pharmacy) because their service professionals can answer specific questions about CU Health Plan coverage. The Customer Care line can be reached at 1-888-964-0121 and is available 24 hours a day, 7 days a week, 365 days a year.
Contact CU’s dedicated CVS Caremark Customer Care line for:
- Questions about coverage or prescription costs.
- Assistance filling a maximum of three 30-day fills before moving to a required 90-day supply via mail order to CVS pharmacies or at a Maintenance Choice pharmacy.
- Assistance locating pharmacies that supply your medications.
- Assistance updating prescriptions with your medical provider.
Contact Employee Services: 1-303-860-4200, option 3 or email benefits@cu.edu
Employee Services benefits professionals are available to assist you with enrollment concerns, obtaining ID cards and resolving issues in a timely manner. Benefits professionals can be reached 9 a.m. to 5 p.m. Monday – Thursday and from 10 a.m. to 5 p.m. Friday.




Add new comment